Thyroid and Hair Loss: Understanding and Taking Action

Summary
Hair loss is a significant source of concern for many individuals. The situation becomes particularly complex when this hair loss is associated with thyroid dysfunction. The statistics are telling: 30 to 40% of patients with thyroid disorders develop some form of alopecia, with prevalence reaching 50% in those with hyperthyroidism.
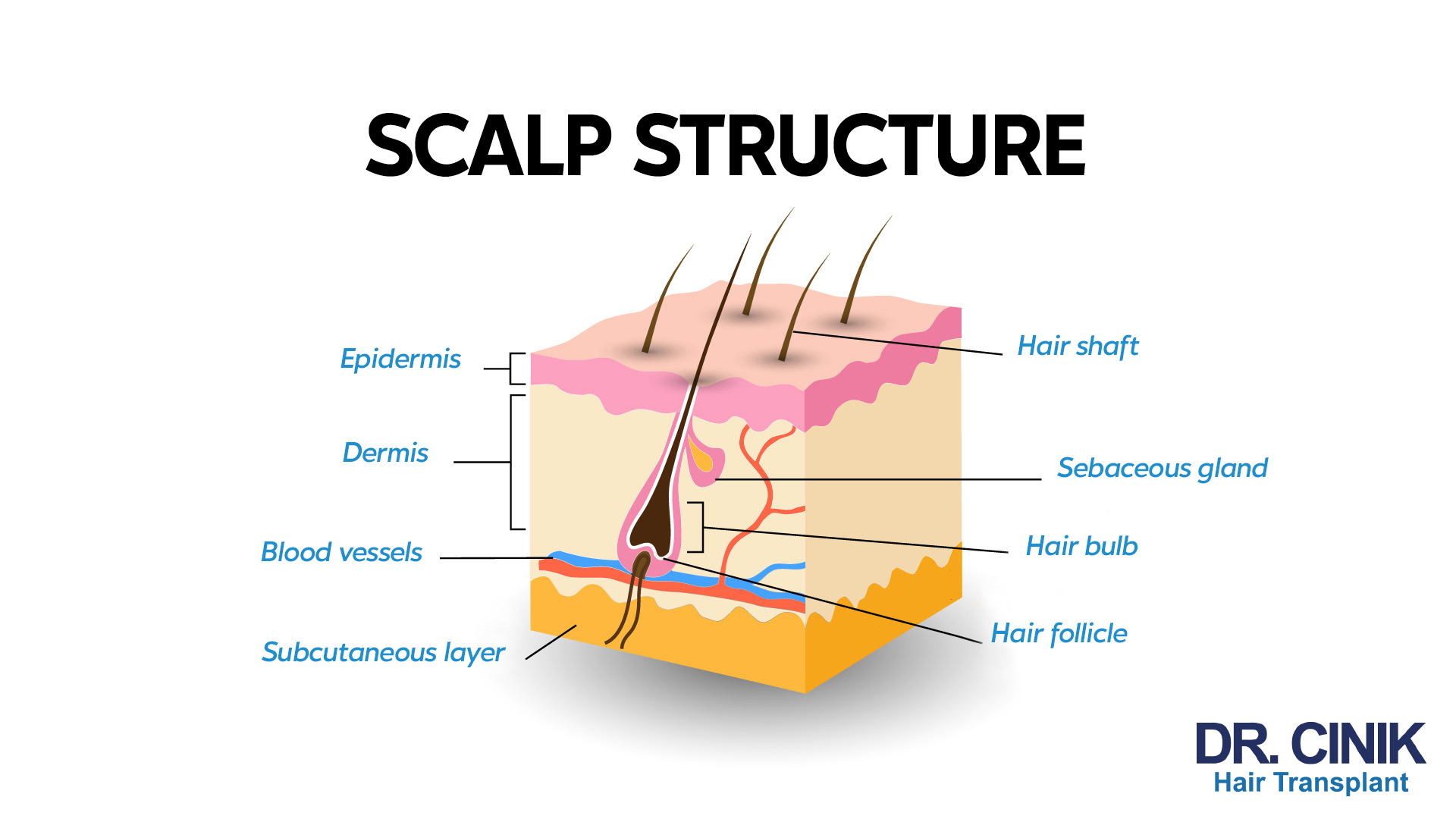
The link between thyroid function and hair health is not coincidental. Thyroid hormones play a crucial role in the growth and maintenance of hair follicles. They regulate the hair life cycle and directly influence hair quality. An imbalanced thyroid can, therefore have a substantial impact on your hair.
Recent scientific advancements have enhanced our understanding of these mechanisms and enabled the development of appropriate therapeutic solutions. Modern diagnostic and treatment techniques, such as those offered by Dr Cinik, present new opportunities for patients facing this issue.
Understanding the Thyroid-Hair Relationship: Mechanisms Revealed
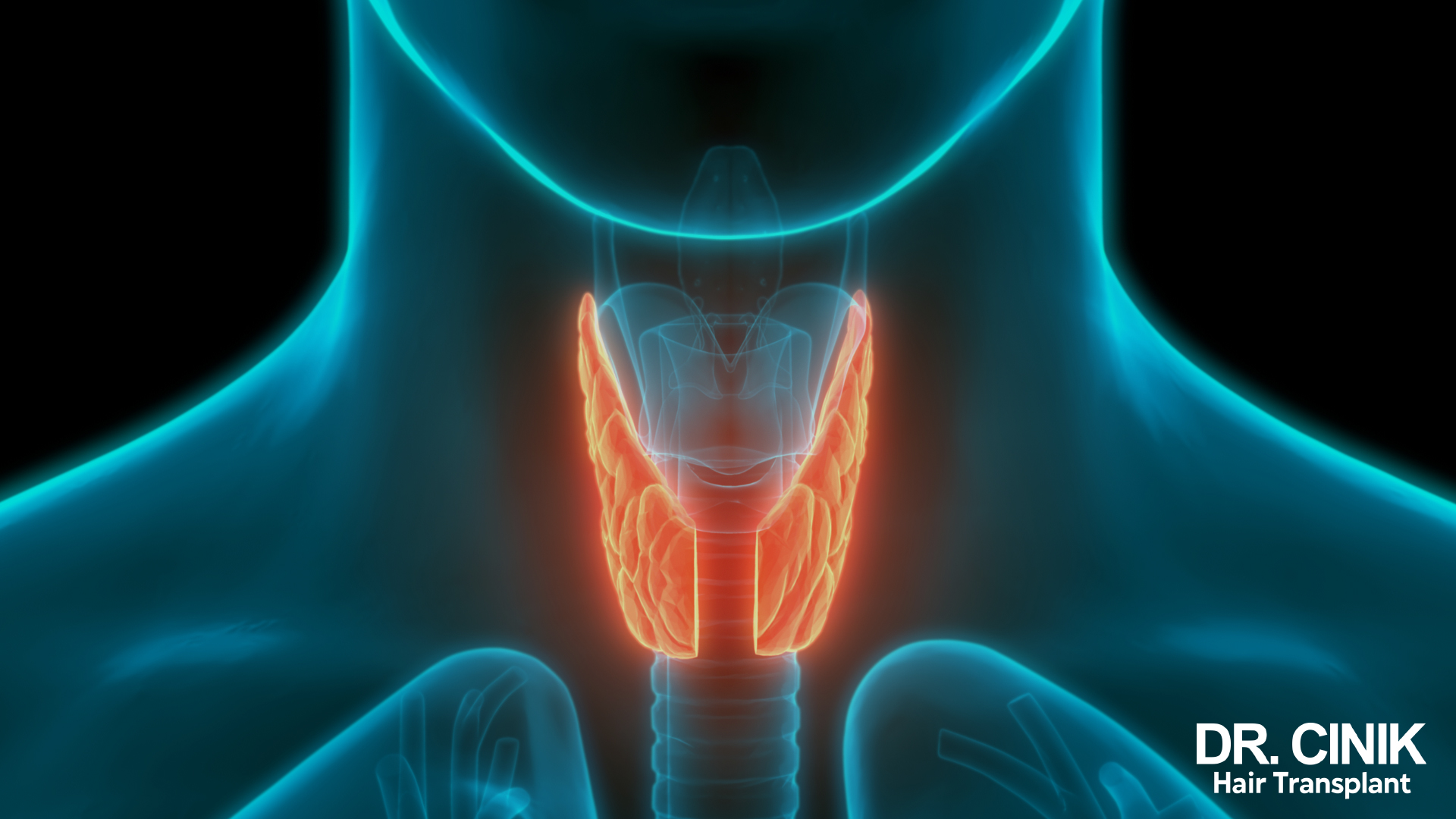
The Essential Role of Thyroid Hormones
The thyroid gland produces two primary hormones: triiodothyronine (T3) and thyroxine (T4). These hormones, regulated by TSH (thyroid stimulating hormone), orchestrate numerous metabolic processes in the body. In hair follicles, they:
- Stimulate hair growth
- Regulate the hair cycle
- Influence hair protein synthesis
- Control the energy metabolism of follicles
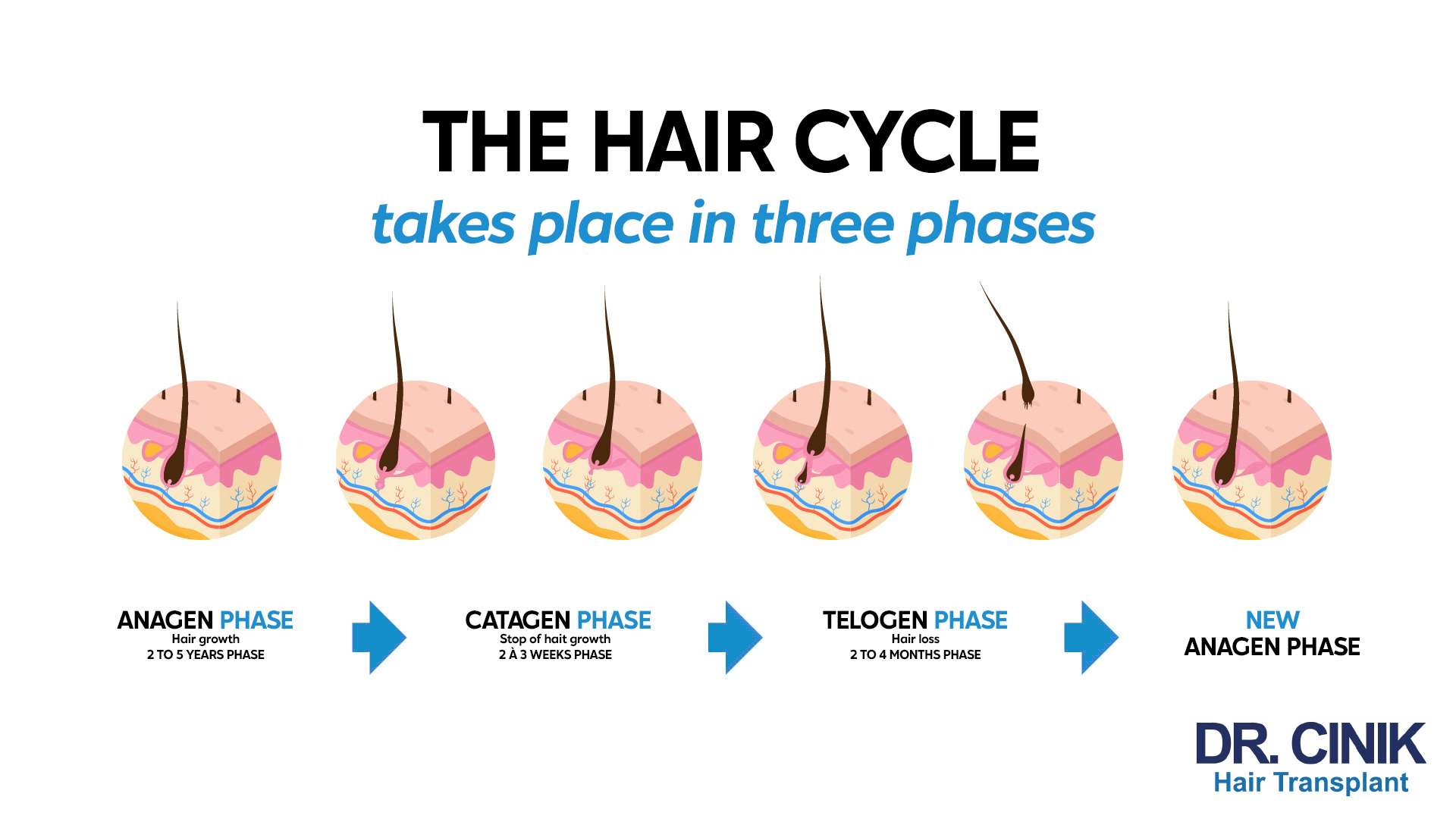
The Hair Cycle: A Delicate Balance
The hair cycle comprises three main phases:
- The anagen phase (2-7 years): A period of active growth when thyroid hormones stimulate cell multiplication and keratin production. Thyroid imbalance can disrupt this crucial phase.
- The catagen phase (2-3 weeks): A transition phase when the follicle enters a resting state. Thyroid hormones regulate the duration of this transition.
- The telogen phase (3-4 months): A period of rest followed by natural hair shedding. Thyroid dysfunction can abnormally prolong this phase.
Thyroid Disorders and Their Impact on Hair
Hypothyroidism: When Hair Weakens
Hypothyroidism, characterised by insufficient production of thyroid hormones, profoundly affects hair health. The resulting metabolic slowdown disrupts the natural hair cycle. Hair follicles, deprived of necessary hormonal signals, struggle to maintain normal growth.
This hormonal deficiency leads to visible changes in the hair. Hair becomes dry, brittle and loses its natural vitality. The texture changes, giving the impression of thinner and less dense hair. One of the most characteristic manifestations is diffuse alopecia, where hair loss occurs progressively across the entire scalp.

Hyperthyroidism: The Acceleration That Weakens
Conversely, hyperthyroidism causes an overproduction of thyroid hormones, with equally harmful consequences for hair. The excessive acceleration of cellular metabolism creates significant stress on hair follicles. This metabolic hyperactivity generates increased production of free radicals, a source of oxidative damage to hair cells.
The clinical symptoms include particularly thin and fragile hair. Hair loses density, not due to slowing down, but because of premature wear of hair fibres. Patients often notice a significant increase in hair loss, accompanied by a change in hair texture.
Autoimmune Thyroid Diseases
- Hashimoto’s disease, the most common form of autoimmune thyroiditis, triggers a chronic inflammatory reaction that can affect hair follicles. The body produces antibodies that attack the thyroid and disrupt the normal hair cycle.
- Graves’ disease has distinct characteristics. This autoimmune condition causes hyperthyroidism, often accompanied by changes in hair texture and widespread hair loss. Patients may also develop other autoimmune manifestations affecting the skin and appendages.

From Consultation to Diagnosis
Accurate diagnosis of thyroid-related hair loss requires a methodical and comprehensive approach. The assessment begins with a thorough clinical examination, followed by targeted biological analyses. Dr Cinik pays particular attention to the patient’s medical history and the progressive changes in their hair.
The cornerstone of diagnosis is the thyroid check-up. TSH values, normally between 0.4 and 4.0 mIU/L, are the first indicator of thyroid dysfunction. Analysis of free T3 (2.3-4.2 pg/mL) and free T4 (0.8-1.8 ng/dL) hormones helps refine the diagnosis. The presence of anti-TPO and anti-TG antibodies reveals a possible autoimmune component.
Dermatological evaluation provides essential additional information. Trichoscopy offers a detailed look at the condition of the scalp and follicles. The pull test assesses the extent of active hair loss, whilst the trichogram analyses hair distribution in different phases of the hair cycle.

Therapeutic Solutions: From Thyroid to Hair
Treatment of Thyroid Disorders
Normalising thyroid function is the first step in treatment. For hypothyroidism, levothyroxine is used to restore adequate hormone levels. The dosage, personalised for each patient, is subject to regular adjustments based on biological monitoring. Hair regrowth generally becomes visible after 3 to 6 months of balanced treatment.
For hyperthyroidism, synthetic anti-thyroid drugs aim to reduce excessive hormone production. Treatment requires close monitoring of side effects and regular assessment of thyroid parameters.
Complementary Dermatological Treatments
A global approach often combines appropriate topical solutions. Minoxidil applied topically, stimulates hair growth and strengthens existing hair. Specific formulations, developed for sensitised scalps, complement the basic treatment.
Targeted supplementation also plays a crucial role. Maintaining optimal iron levels (above 70 μg/L), providing zinc and B vitamins, and sulphur-containing amino acids support hair health during the recovery phase.

Hair Transplants: A Solution for Stabilised Cases
Hair transplants represent a lasting solution for patients whose thyroid function has stabilised. Dr Cinik recommends waiting at least one year for documented thyroid stability before considering this procedure. Prerequisites include normalised TSH and the absence of active inflammation.
Dr Cinik offers several modern surgical techniques, each tailored to the patient’s specific needs. Conventional FUE allows for precise follicular extraction with minimal scarring. The FUE Sapphire technique, using sapphire micro blades, offers greater precision and optimal healing. The particularly innovative DHI method allows direct implantation of grafts, maximising density while reducing recovery time.
Post-transplant follow-up is particularly important in patients with a history of thyroid disease. Close monitoring of hormonal balance continues in parallel with monitoring of regrowth, which generally lasts for 12 to 18 months.

Practical Advice and Long-term Follow-up
Monitoring and Prevention
A personalised follow-up programme is always necessary to maintain results. Regular thyroid checks enable hormone treatment to be adjusted quickly if necessary. Periodic dermatological assessment ensures early detection of any complications.
Optimising Your Daily Routine
Hair health requires special attention every day. Gentle hair care products specifically formulated for fragile hair help preserve its integrity. Styling techniques should avoid excessive traction on the roots.
Diet plays a fundamental role in hair health. A balanced diet, rich in quality proteins, omega-3, and antioxidants, supports hair growth and quality. Dr Cinik particularly recommends foods that promote thyroid balance.

Conclusion
The relationship between thyroid and hair health illustrates the complexity of the biological mechanisms involved. Early diagnosis and comprehensive treatment are key to therapeutic success. Once thyroid balance has been restored, hair health generally significantly improves.
Technological advances in hair transplantation, combined with an in-depth understanding of thyroid-hair interactions, now offer personalised, long-lasting solutions. Dr Cinik and his team are committed to guiding each patient through the hair restoration process, taking into account the specific characteristics of their thyroid condition.
Successful treatment is based on a holistic approach, combining hormone balancing, appropriate hair care, and lifestyle changes. This therapeutic synergy, supported by regular monitoring, optimises long-term results.
References
Vincent, M., & Yogiraj, K. (2013). A descriptive study of alopecia patterns and their relation to thyroid dysfunction. International Journal of Trichology, 5(1), 57-60. https://pmc.ncbi.nlm.nih.gov/articles/PMC3746235/
van Beek, N., Bodó, E., Kromminga, A., et al. (2008). Thyroid hormones directly alter human hair follicle functions: anagen prolongation and stimulation of both hair matrix keratinocyte proliferation and hair pigmentation. The Journal of Clinical Endocrinology & Metabolism, 93(11), 4381-4388. https://pubmed.ncbi.nlm.nih.gov/18728176/
Contreras-Jurado, C., Lorz, C., García-Serrano, L., Paramio, J. M., & Aranda, A. (2015). Thyroid hormone signaling controls hair follicle stem cell function. Molecular Biology of the Cell, 26(7), 1263-1272. https://pmc.ncbi.nlm.nih.gov/articles/PMC4454174/
Stenn, K. S., & Paus, R. (2001). Controls of hair follicle cycling. Physiological Reviews, 81(1), 449-494. https://pubmed.ncbi.nlm.nih.gov/11152763/
Alessandrini, A., Bruni, F., Piraccini, B. M., & Starace, M. (2021). Common causes of hair loss-clinical manifestations, trichoscopy and therapy. Journal of the European Academy of Dermatology and Venereology, 35(3), 629-640. https://pubmed.ncbi.nlm.nih.gov/33290611/
Lee, S., Lee, H., Lee, C. H., & Lee, W. S. (2019). Comorbidities in alopecia areata: A systematic review and meta-analysis. Journal of the American Academy of Dermatology, 80(2), 466-477. https://pubmed.ncbi.nlm.nih.gov/30031145/
Bin Saif, G. A. (2016). Severe subtype of alopecia areata is highly associated with thyroid autoimmunity. Saudi Medical Journal, 37(6), 656-661. https://pmc.ncbi.nlm.nih.gov/articles/PMC4931647/
Mubki, T., Rudnicka, L., Olszewska, M., & Shapiro, J. (2014). Evaluation and diagnosis of the hair loss patient: part II. Trichoscopic and laboratory evaluations. Journal of the American Academy of Dermatology, 71(3), 431-e1. https://pubmed.ncbi.nlm.nih.gov/25128119/




