Can Anyone Get a Hair Transplant? The Complete List of Hair Transplant Contraindications

Summary
Hair transplantation is a surgical technique used to treat certain types of alopecia, including androgenetic alopecia, by removing healthy hair follicles from a donor area at the back of the head and re-implanting them in balding areas. When performed by a qualified surgeon, the results are long-lasting in most cases. However, some notable contraindications to hair transplantation should be noticed. This article provides an exhaustive list of all the potential contraindications to hair transplantation for patients to assess their eligibility for the procedure.

Medical contraindications to hair transplantation
Some pre-existing medical conditions may be absolute or relative contraindications for hair transplantation.
Autoimmune diseases
Many autoimmune diseases such as lupus, rheumatoid arthritis, ankylosing spondylitis, vitiligo, psoriasis and alopecia areata are contraindications for hair transplantation. The patient’s overactive immune system may identify the implanted hair grafts as foreign bodies and attack them, likely leading to the failure of the transplant.
An in-depth consultation with the surgeon is necessary to evaluate risks on a case-by-case basis. If the autoimmune condition has been stabilised for several years under medical treatment, a hair transplant procedure may be considered.

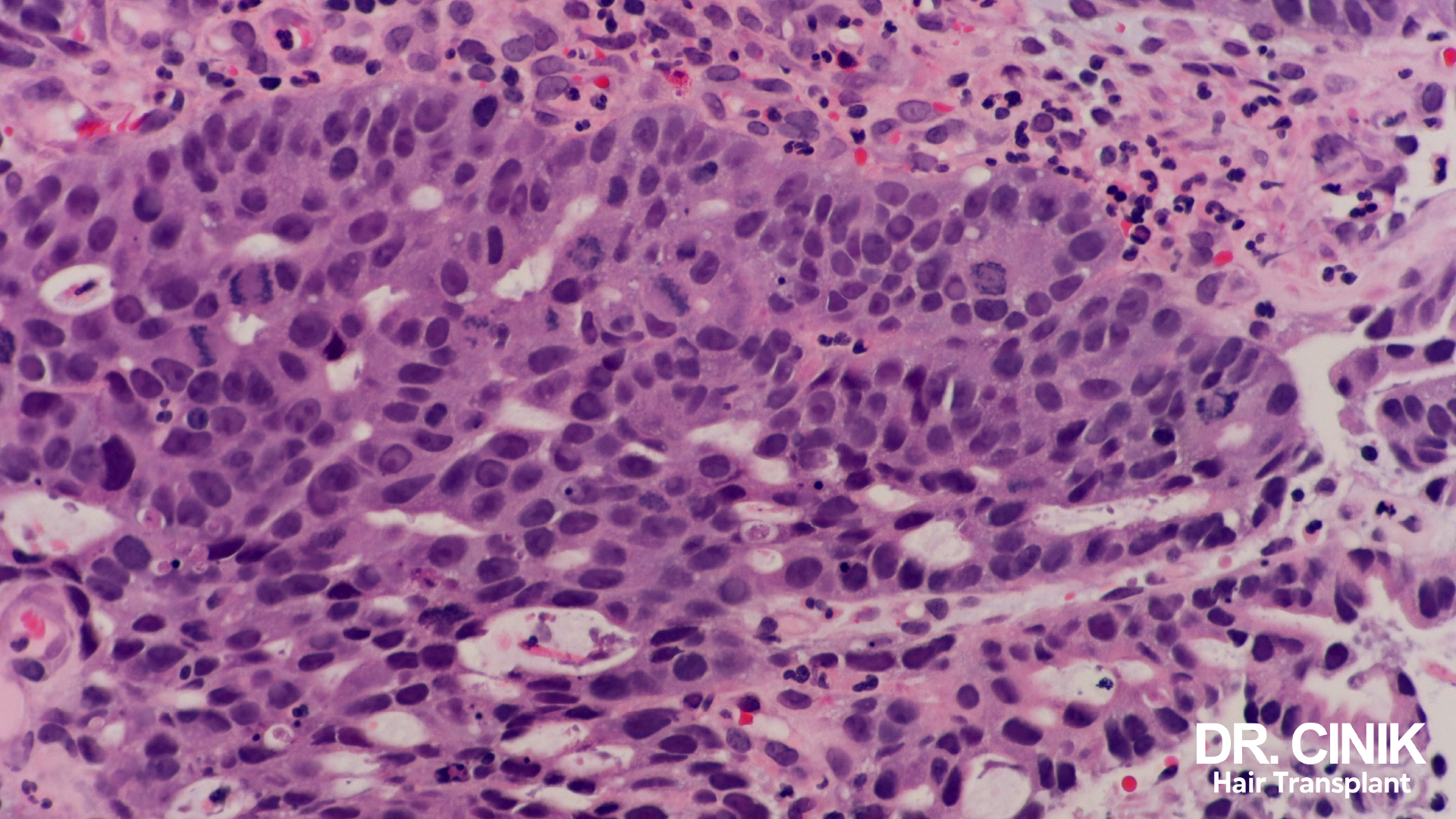
Recent history of cancer
Patients with a history of cancer, particularly of cutaneous or haematological origin, must check with their oncologist that sufficient time has elapsed since the end of their cancer treatment. Chemotherapy and radiotherapy are very aggressive treatments that can have a lasting effect on skin tissue quality and the ability of hair follicles to regenerate and heal properly. A minimum period of 12 to 24 months after finishing chemotherapy or radiotherapy is generally recommended by specialists before considering a hair transplant procedure.

Endocrine disorders
Various endocrine system disorders can represent a risk for hair transplantation if not properly managed beforehand:
- Diabetes, especially when uncontrolled, is likely to alter scalp vascularisation, compromising the viability of hair follicle grafts.
- Thyroid disorders such as hypothyroidism or uncontrolled hyperthyroidism that are not adequately treated can impact skin and hair cell vitality and regeneration. This can negatively affect hair graft regrowth quality after transplantation.
- Adrenal hypercortisolism, also known as Cushing’s syndrome, can lead to skin thinning and tissue fragility, interfering with graft healing.
- Hyperandrogenism from ovarian or adrenal origin leads to excessive production of androgenic hormones like testosterone in women. This androgen excess can cause abnormal hair growth (hirsutism) or virilisation symptoms (deepened voice, male-pattern baldness, etc.). This hormonal imbalance disrupts the hair cycle and accelerates hair loss. Regulating this androgen excess with appropriate treatment is recommended before considering a hair transplant for optimal viability.
- Insulin resistance associated with dyslipidemia as part of metabolic syndrome also alters scalp blood microcirculation and potentially the viability of implanted hair follicles.
- Severe obesity can result in poorer wound healing and requires technical precautions during the procedure.

Heart and vascular diseases
Certain cardiovascular conditions may temporarily contraindicate hair transplantation. These diseases can disrupt blood flow and oxygen supply to the scalp area, compromising hair follicle grafts’ proper implantation and survival.
This is particularly the case for:
- Severe high blood pressure that is uncontrolled by medication, with levels permanently above 160/100 mmHg. Better control of hypertension is necessary before a hair transplant.
- The presence of lower limb arterial disease often reflects systemic vascular damage. This poor circulation can impact scalp vascularisation and threaten the viability of implanted grafts.
- Advanced (Stage 3 or 4) heart failure requires the patient’s general health to be stabilised before considering an elective procedure such as a hair transplant.
- The recent occurrence of a heart attack or stroke may necessitate postponing the hair transplant procedure for a few months.
Coagulation disorders
Certain coagulation disorders preclude hair transplantation:
- Hemophilia and other diseases where the blood fails to clot properly due to deficiencies in specific coagulation factors.
- You are taking blood thinners such as anticoagulants or platelet aggregation inhibitors. These alter normal blood clotting during surgery.
- Diseases with abnormal platelet counts (thrombocytopenia, thrombocytosis).
- Severe anaemia with deficient haemoglobin levels (< 8 g/dL).
- Sickle cell disease is a blood disorder that can disrupt coagulation.
In all these cases, there is an increased risk of excessive bleeding during surgery, which makes hair transplantation inadvisable.
Immunocompromised patients
Certain situations leading to weakened immunity pose risk factors for hair transplantation:
- Uncontrolled HIV infection with very low CD4 T-cell counts (< 200/mm3).
- Rare genetic immune deficiencies.
- Surgical spleen removal (splenectomy).
These patients are more prone to infections. It is advisable to postpone hair transplant procedures until their immune function has been restored.
Psychological or psychiatric contraindications
Certain psychological or psychiatric conditions represent relative or absolute contraindications to consider before hair transplantation.

Psychological or psychiatric contraindications
Certain psychological or psychiatric conditions represent relative or absolute contraindications to consider before hair transplantation.
Severe body image disorders
Several psychological disorders lead patients to develop a distorted or obsessive perception of their physical appearance:
- Body dysmorphic disorder: an obsessive preoccupation with an imagined or highly exaggerated physical flaw. These patients view their baldness as shameful, terrifying, and socially ruinous. However, post-surgery, new defect areas emerge, leading to chronic dissatisfaction.
- Certain psychotic disorders like schizophrenia, delusional disorders or melancholic depression. Hair transplantation is contraindicated in these cases.
- Obsessive-compulsive disorders (OCD), such as ritualistic checking behaviours and trichotillomania (compulsive hair pulling), require treatment before considering hair transplants.
Depressive disorders
The presence of severe depressive episodes, especially when accompanied by suicidal ideation, is a relative contraindication for hair transplantation. It is advisable to stabilise the patient’s mood and alleviate depressive symptoms before contemplating elective cosmetic surgery. Depression can otherwise undermine motivation to comply with post-operative care requirements.
Addiction to cosmetic procedures
Some patients can develop an addiction, meaning a psychological dependence, to various cosmetic surgical procedures (facelifts, fillers, etc.) or dermatological treatments. They compulsively seek consultations and remain chronically dissatisfied, regardless of the procedures performed. For these patient profiles, further cosmetic procedures are inadvisable.
Unrealistic expectations
Some patients harbour overly optimistic expectations regarding the scalp density and coverage realistically achievable from a hair transplant. Dialogue at consultation is necessary to recalibrate patient expectations to reasonably anticipated outcomes. The patient must agree with the surgeon regarding feasible results.
Lifestyle-related contraindications
Certain behaviours and lifestyle habits may also represent relative or absolute contraindications for hair transplantation.

Heavy smoking
Smoking more than one pack per day alters blood microcirculation. This impacts the viability of implanted hair grafts, which require adequate oxygen supply to heal. Additionally, the patient must stop smoking for at least two weeks postoperatively.
It is, therefore, strongly advised for smokers to initiate the quitting process a few months before undergoing hair transplant surgery.
Alcoholism
Likewise, excessive and chronic alcohol intake beyond recommended limits can impair scalp vascularisation and graft healing. This level of drinking should be drastically reduced when preparing for hair transplant surgery. Patients should also abstain from alcohol intake for 3 weeks after the hair transplant.
Temporary contraindications
Certain situations or conditions may warrant temporarily postponing hair transplant procedures.

Pregnancy
It is advisable to postpone hair transplantation if you are actively pregnant or planning pregnancy within one year following the surgery. Hormonal changes and increased vascularisation during pregnancy can interfere with graft healing and optimal development.
Intense emotional stress
Likewise, postponing hair transplants may be preferable if the patient is enduring intense psycho-emotional stressors: bereavement, separation, job loss, etc. These life events around the surgical timeframe can complicate the immediate post-operative recovery.
Contraindications related to baldness stage

Unstable baldness pattern
Waiting for hair loss pattern stabilisation before considering hair transplantation is necessary. Androgenetic alopecia generally stabilises between the ages of 25 and 30. For those prone to premature baldness, Minoxidil is recommended to slow alopecia progression while waiting for the pattern baldness to stabilise.
Advanced baldness
Patients with baldness reaching stage 6 on the Norwood scale are no longer candidates for hair transplantation due to insufficient donor hair reserves.